Disclosure: This post contains affiliate links, meaning that if you are to make a purchase via these links, the blog author receives a small commission. This helps to fund the mission of Spencer’s Whole Foods Plant Based Eats and Treats, which is to be on the frontier in the fight against obesity and chronic disease in Trinidad & Tobago by contributing to changing the dietary environment of the nation.
As an Amazon Associate, the blog author earns from qualifying purchases.
NCDs and the 2024 Trinidad & Tobago Budget
On October 30th 2023, a letter to the editor of the Trinidad Express by international public health consultant Dr Kenwyn Nicholls titled ‘Have we dropped the ball on NCDs?’ was published.
This blog post is a response to that question.
In his letter, Dr Nicholls pointed to the 2024 Budget debate contribution by Independent Senator Sunity Maharaj, in which she noted that the ‘Budget failed to address the country’s leading killer, non-communicable diseases (NCDs).
@sunitymaharaj and her initial thoughts on the 2024 Trinidad & Tobago Budget speech#2024Budget pic.twitter.com/v9FTo8GP4S
— Spencer's Whole Foods Plant Based Eats and Treats (@SpencersWFPB) March 26, 2024
In the Budget speech, there were only three sentences in which the Minister of Finance addressed NCDs:
“We have adopted a multi-disciplinary approach for sustainable solutions towards preventing, managing and controlling the burden of mobility, mortality and disability due to non-communicable diseases. We seek to ensure that the population can reach the highest attainable standards of physical and mental health, quality of life and productivity at every age. We are committed to ensuring that those diseases will no longer be a barrier to well-being and socioeconomic development in the country.”
The next logical question should be how these ‘sustainable solutions’ could be achieved.
National Strategic Plan for NCDs
Dr Nicholls also mentioned the Ministry of Health document “National Strategic Plan for
the Prevention and Control of Non-Communicable Diseases: Trinidad and Tobago
2017 – 2021”. In it, he highlighted the envisioned phased implementation of the plan in three phases. Phase 1 was supposed to be implemented in one year, and one of the action items that was to be implemented was a “dedicated NCD unit”. It was to be a multisectoral team and the primary objectives of this dedicated NCD unit were to
- Develop and start implementing the action plans for Phase 1
- Develop the Monitoring and Evaluation Framework
After perusal of Dr Nicholls’ letter and the Ministry of Health document referenced earlier, it saddens me to say that I can answer the question posed by Dr Nicholls in the affirmative:
We have dropped the ball on NCDs. And there are many examples which I can draw from to show this. However, in this letter, I will show two examples.
Establishment of 'Dedicated NCD Unit'
To begin, the National Strategic Plan was due to start in 2017 with the dedicated NCD unit and the rollout of Phase 1 action plans. This was outlined on page 32 of the document:
“A dedicated NCD Unit will be established with a multisectoral team and reporting to the Permanent Secretary. Among the first actions for the Unit will be the development of an Action Plan for year 1 and the Monitoring and Evaluation Framework.”
However, the NCD unit’s Director position wasn’t posted until 2022 and was only filled by Dr Maria Clapperton in April 2023.


From recent memory, Dr Clapperton has been the only person representing this NCD unit in meetings and interviews. Isn’t the NCD unit supposed to be a multisectoral team? Therefore, this NCD unit should have representatives from different sectors and not just one person speaking on behalf of the whole NCD unit. There isn’t much clarity as to who are the senior members that make up this ‘multisectoral’ NCD unit and it is my view that these members from different sectors should be more visible in the eyes of the population. The Phase 1 action plans proposed by the National Strategic Plan document is a large undertaking; too much for one person.
Hypertension - how is being addressed in Trinidad & Tobago?
When one looks at the Action Plans in the document, anyone who is even slightly versed in the field of public health, especially concerning chronic disease, will know that the Action Plans, if implemented properly, will make a major dent in the NCD trend and will shift the health of the population for the better in a tangible manner.

To explain what I mean, first some context. Trinidad and Tobago has a rate of hypertension that is higher than both the Caribbean average and the global average.
According to Dr Abdul Hamid, Primary Care Physician 2 of the NCRHA, large-scale public screenings have revealed a 50% hypertension rate!
Dr Abdul Hamid, primary care physician of the @NCRHATT, gives some statistics for Trinidad & Tobago regarding hypertension or high blood pressure#hypertension #highbloodpressure #TrinidadandTobago pic.twitter.com/Irbj4SMBpN
— Spencer's Whole Foods Plant Based Eats and Treats (@SpencersWFPB) March 28, 2024
A 2008 scientific review by He and MacGregor titled ‘A comprehensive review on salt and health and current experience of worldwide salt reduction programmes’ talked about salt consumption and its strong link to hypertension or elevated blood pressure
Hypertension mainly causes damage through its effect on cardiovascular disease (CVD), which is the major cause of death worldwide. Worldwide elevated blood pressure, elevated cholesterol and smoking account for over 80% of CVD.
However, elevated blood pressure is the single most important cause, responsible for 62% of strokes and 49% of coronary heart disease (CHD). What is also of note is there is a continuous relationship between blood pressure and cardiovascular disease, beginning at 115/75 mmHg.
A large number of scientific studies have been conducted, all of which support the concept that salt intake is the major factor in increasing blood pressure in any given population.

Salt Intake Recommendations of Major Health Organisations
The World Health Organisation recommends a maximum sodium intake of 2000 mg, which translates to 5g of salt or just under one teaspoon. The American Heart Association’s ideal sodium recommendation is 1500 mg or just under ¾ teaspoon of salt.
CARPHA estimates Caribbean salt intake to range between 9-12 g. However, in Trinidad & Tobago, there is no established figure of population salt intake.
What is Trinidad and Tobago's salt intake?
He and MacGregor made this comment in their review:
“It is important that each country in the world determines what its salt intake is and where are the major sources of salt in the diet, and then implements a strategic approach to lowering salt intake in the population to the target level”
Ironically, Action Plan 1.3.2 in the National Strategic Plan was as quoted:
“Establish baseline for population sodium and Trans fat intake.”
To establish the sodium intake of the population, one or more studies must be done, the same for trans fats. My research efforts have yielded no such study/studies for the Trinidad and Tobago population. This is one of the many Phase 1 action plans that were not done between 2017 and 2021 and still have not been done in 2024.
There is a saying by management theorist Peter Drucker which says, “What gets measured gets improved”. It is unbelievable, given Trinidad and Tobago’s blood pressure statistics, that there hasn’t been a public conversation about acquiring data about the population’s salt intake when it is well-known that salt intake and blood pressure are very closely associated, as seen in the video below.
Trinidad & Tobago and the INTERSALT study
Some things to note about the 1988 INTERSALT study referenced in the video above.
- Trinidad and Tobago was one of the 32 countries involved in the study.
- The centre in Trinidad in which the study was conducted was the Plymouth Health Centre.
- The mean urinary sodium excretion of the Trinidad & Tobago cohort was 117.3 mmol in 24hrs. This equates to almost 2700 mg of sodium excretion.
- The prevalence of hypertension in the Trinidad & Tobago cohort of the INTERSALT study was 18%.
- This was higher than
- Argentina
- India
- Japan
- Kenya
- Mexico
- Brazil
- Papua New Guinea
- China
- South Korea
- (Fmr.) Soviet Union
- Spain
- Taiwan
- (Fmr.) West Germany
- 2700 mg was the average sodium excretion of the cohort in the Barbados salt study. Barbados has a hypertension prevalence of 42%.
Salt control in other countries
Barbados
By contrast, the Barbados Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2015–2019, also outlined the reduction of salt as one of its priorities. This is because hypertension is also a public health priority in Barbados, where it is estimated that 42% of its population is hypertensive.
However, Barbados carried out a study on salt intake in their population, which estimated that their sodium intake was 2700 mg a day, which translated to over 1 teaspoon of salt. This data at baseline will give the health and legislative authorities a platform to establish a salt reduction strategy. Of note, in 2023, Prime Minister Mia Mottley spoke about an impending sodium tax.
If Barbados makes good on its promise of a sodium tax, it will join the growing list of countries that have implemented legislative action on high-salt foods and salt in general. This will include the UK, Finland, Canada, Hungary, Japan and others.
@miaamormottley in the 2023 Barbados budget presentation highlights the scourge of NCDs plaguing the population and the impending sodium tax implementation pic.twitter.com/ETK830InUL
— Spencer's Whole Foods Plant Based Eats and Treats (@SpencersWFPB) March 28, 2024
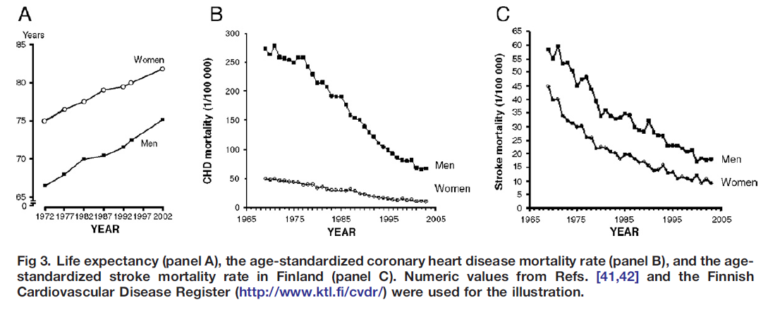
Finland
In Finland, sodium intake was 12 g per day in 1979. In 2002, it was measured at 9g per day. This was accompanied by a fall of over 10mmHg in both systolic and diastolic BP, a pronounced decrease of 75–80% in both stroke and mortality due to heart disease, and a remarkable increase of 5–6 years in life expectancy.
Conclusion
There is nothing to suggest that these health improvements cannot happen in Trinidad and Tobago. But the present health and legislative authorities need to do the heavy, tedious work for this to take place. Will they muster the gumption to do this? Or will NCDs continue to, as Dr Asante Le Blanc says “a whole lot of talk and no action”?
Will the Health Ministry and by extension, the Government, continue to drop the ball?